Electronic medical records (EMRs) and electronic health records (EHRs) play an integral role in healthcare data management today. However, medical and healthcare professionals still encounter confusion regarding the key differences between these technologies. Developing a clear understanding of the differences between EMR and EHR can empower physicians and clinics to make informed decisions when adopting health information systems. This article provides a comprehensive breakdown of the distinctions across functionality, data sharing capabilities, patient engagement features, and implementation considerations.
Key Functionality Differences
At their core, the difference between EHR and EMR systems lies in their divergent functional scopes:
EMRs focus narrowly on the electronic documentation of health information within a single organization, like a hospital or physician’s clinic. EMRs function as digital replacements for paper-based medical records.
EHRs provide integrated and shareable patient health data from across multiple care settings. EHRs offer a broader, more comprehensive view of a patient’s medical history by linking data from different healthcare providers.
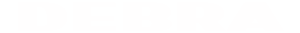
According to estimates, while 96% of healthcare organizations leverage some form of digital recordkeeping through EMR adoption, only 76% have transitioned toward multi-organization health data sharing through EHR systems.
Interoperability and Data Sharing Capabilities
Interoperability enables seamless health data exchange across organizations. This capacity for data fluidity confers multiple benefits:
- Prevents redundant testing – By aggregating patient diagnostic testing histories across providers, repeat procedures are avoided, saving costs.
- Improves care coordination – Data sharing allows different facilities like hospitals, clinics and pharmacies to synchronize treatment plans, enhancing care continuity as patients transition between settings.
- Upgrades clinical decision making – Comprehensive health profiles from interoperable records integrate patient medical, medication, laboratory, immunization and allergy histories into one view for precise care.
- Bolsters public health monitoring- Widespread interoperability supplies rich datasets for public health agencies to detect disease outbreaks early and track population health trends.
However, significant obstacles continue to plague interoperability:
- Data blocking concerns – Business or technical barriers deliberately raised by EHR vendors to choke competitor access to patient data for enhanced market control.
- Limited health information exchange – Only 53% of physicians can easily integrate outside patient health data into EHR workflows, restricting true interoperability.
- Standards development challenges- Competing technological standards across proprietary health IT systems delay consensus on uniform data exchange frameworks.
Nevertheless, the 21st Century Cures Act aims to enforce EHR vendor cooperation on data sharing while governing agencies explore technological solutions to achieve seamless nationwide interoperability by 2030.
Features for Patient Engagement
EHRs usher in advanced digital features for patients and caregivers encompassing 4 key areas:
- Streamlined Administrative Tasks
Patient portals integrated with backend EHRs simplify essential health management workflows through self-service:
Schedule clinical visits, prescription refills or lab testing online without calling the clinic.
Complete pre-appointment check-in digitally via apps for a fast touchdown at the facility.
Reduce wait-times and errors by completing electronic intake forms ahead of appointments.
- Health Information Accessibility
Patients can securely look up their consolidated medical records including test results and doctor recommendations from any device. Such perpetual access empowers patients to be active health managers.
- Care Team Communications
Message care providers about health concerns, medication queries or side-effects securely without time lags. Some portals even offer patient communities to exchange peer support.
- Personal Health Tracking
Digital symptom journals, medication logs and wearable health data syncing allows patients to record experiences between visits. This bridges care transitions and furnishes personalized insights.
With these self-service functionalities at their fingertips, patients gain greater autonomy over their health journeys while clinics leverage EHR connectivity to deliver seamless virtual care capabilities.
Implementation Considerations for Medical Practices
The decision of whether to adopt an EMR-only or make the transition to a full-fledged EHR system depends on several medical practice-specific parameters:
Regulatory Compliance
Medical records management bears tremendous regulatory oversight requiring healthcare software acquisitions to factor in ongoing compliance costs:
- HIPAA regulation violations carry penalties spanning hundreds of thousands of dollars annually, making security and privacy necessities.
- Promoting Interoperability rules mandate specific EHR functionalities to qualify for federal incentive payments. Software must align with these latest interoperability, safety, and data usage standards.
Integration with Existing Healthcare IT Systems
With 40% of providers struggling with integrating new technologies into workflows, EHR implementations warrant careful evaluations of organizational readiness for change management:
- Will staff productivity suffer under new software workflows?
- Can claims and billing be accurately tracked during system transitions?
- Have backup plans been instituted in case of electronic record-keeping failures?
Getting integration right promises tremendous efficiency dividends, with seamless EHR incorporations yielding 30% fewer claim denials and 20% greater staff productivity.
Frequently Asked Questions
What are the primary differences between EMR and EHR systems?
The core distinction lies in scope. EMRs focus narrowly on digital documentation within a single organization. EHRs integrate and share patient data from across multiple providers to enable coordinated care delivery.
Should I transition from just EMR to a full-fledged EHR system?
If care coordination across healthcare facilities is a priority, then yes. By aggregating patient data histories across providers, EHRs vastly improve clinical decision support through comprehensive health records. Achieving this interoperability requires adopting certified EHR systems.
What should I evaluate when selecting an EMR or EHR?
Beyond meeting care delivery needs, medical practices should ensure regulatory compliance for data safety and interoperability while accounting for cost-benefit tradeoffs. Moreover, personalized workflows, data accuracy, backup reliability and user experiences warrant careful assessment during pre-implementation.
Conclusion
In closing, grasping the intricacies between EMR and EHR is imperative for medical and healthcare professionals navigating a data-driven healthcare landscape. While EMRs provide digitized documentation, transitioning toward robust and interoperable EHRs can profoundly upgrade patient experiences, care coordination, cost savings and regulatory compliance for modern medical practices.